
How can early warnings score improve care?
Wissensdatenbank Technologie Datenmanagement & Digitalisierung Mensch Patient*innenzentrierung B.1: Wearable-basiertes kontinuierliches PatientInnen-MonitoringIn the previous article, we explored the challenges hospitals face in the timely detection of patient deterioration and the validation of effective risk-stratification systems. Changes in vital signs are often the first indicators of abnormal physiological changes in the body. Yet, despite their importance in communicating deterioration, many studies have highlighted that vital signs are not regularly measured, documented, or adequately interpreted in hospital wards.
How can early warnings score improve care?
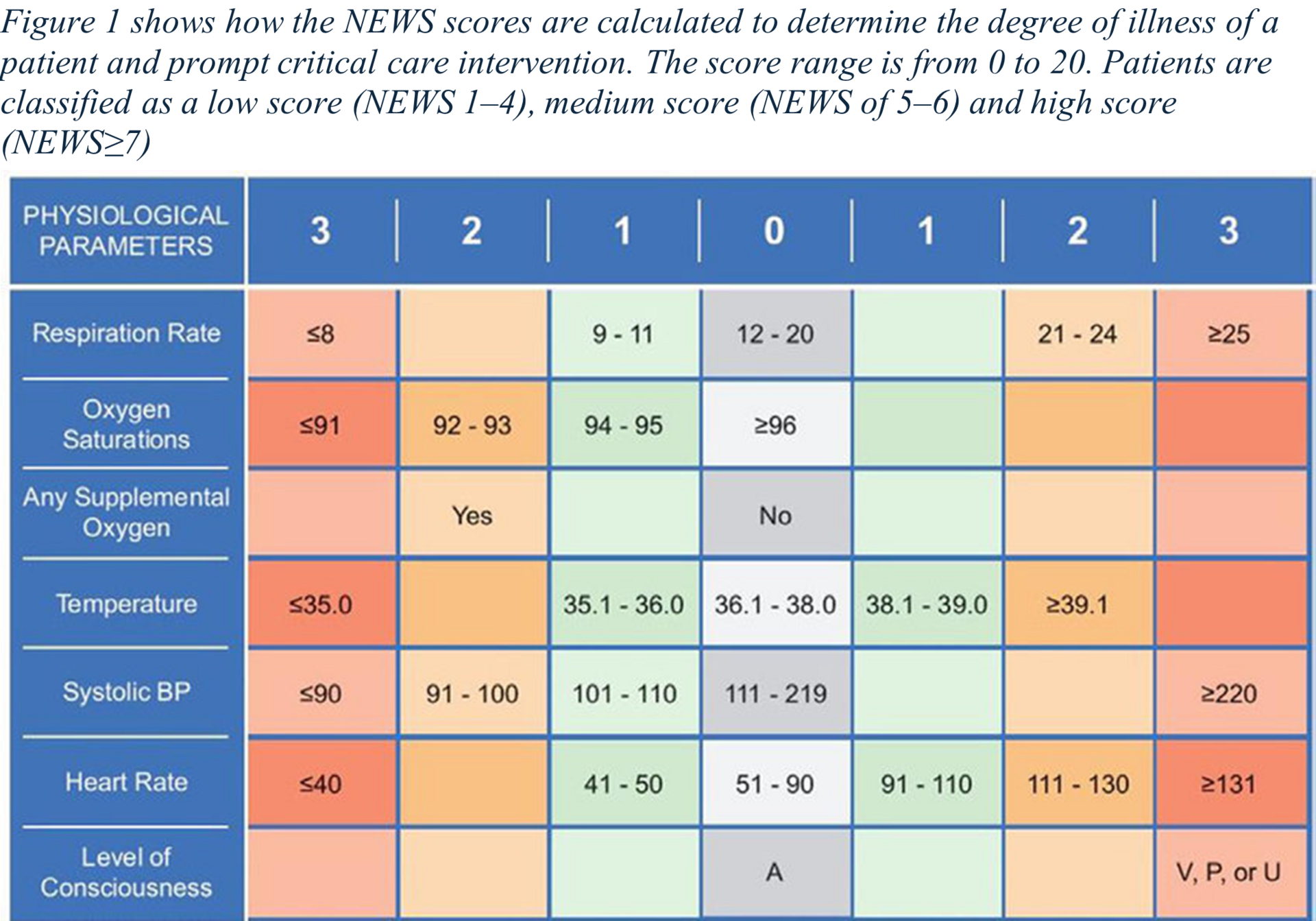
In the previous article, we explored the challenges hospitals face in the timely detection of patient deterioration and the validation of effective risk-stratification systems. Changes in vital signs are often the first indicators of abnormal physiological changes in the body. Yet, despite their importance in communicating deterioration, many studies have highlighted that vital signs are not regularly measured, documented, or adequately interpreted in hospital wards. This suboptimal care, resulting from infrequent monitoring and the misinterpretation of vital signs, can prevent early identification of deterioration and delay transfer to ICU, resulting in preventable adverse events that compromise patient safety. Early Warning Scores (EWS) were introduced as a way to provide an objective and standardized approach for assessing a patient's risk of deterioration, improving the recognition of abnormal vital signs. EWS systems use routine measurements of heart rate, blood pressure, respiratory rate, temperature, and consciousness level, with each parameter assigned a score from 0 to 3. The total score reflects a patient's risk level, helping to track their condition and trigger timely action when necessary. For instance, while an elevated temperature might suggest infection, it is often accompanied by an increase in heart rate and respiratory rate. Individually, these changes may be subtle, but when aggregated through EWS, they become more pronounced and actionable.
Standardizing EWS: The National Early Warning Score (NEWS)
Over the years, many EWS algorithms have been developed, each accompanied by an escalation protocol that dictates how frequently patients should be monitored and what actions should be taken. Among these, the National Early Warning Score (NEWS) is the most widely used. Developed in 2012 by the Royal College of Physicians in the UK, NEWS standardized the recording of seven key vital parameters: respiratory rate, heart rate, systolic blood pressure, oxygen saturation, temperature, and the Alert-Verbal-Pain-Unresponsive (AVPU) scale for consciousness levels. Each parameter is scored between 0 and 3 based on its deviation from normal ranges, with higher scores indicating more urgent risk. A low NEWS score may indicate that regular monitoring is sufficient, while a higher score can trigger rapid intervention, such as calling a response team. Since its introduction, NEWS has been validated and widely implemented across healthcare systems globally, leading to improved outcomes in detecting and responding to patient deterioration.
From Observation Charts to Digital EWS
Traditionally, hospitals rely on observation charts where vital signs are periodically recorded manually to alert staff of potential deterioration. These charts are often designed according to the subjective preferences of healthcare professionals at individual institutions, leading to a lack of standardization. To address this, as mentioned, standardized EWS systems like NEWS, have been implemented globally to help nurses and doctors interpret vital signs more effectively in a more objective way. These systems created a common language for healthcare teams, ensuring that patient deterioration is recognized promptly and appropriately escalated. Observation systems typically fall into three categories:
- Single- and multiple-parameter systems: These compare vital signs against pre-set thresholds to determine if any parameter has reached critical levels.
- Aggregate weighted scoring systems: These assign scores to individual vital signs based on how much they deviate from normal ranges.
- Combination systems: These integrate both aggregate scores and single- or multiple-parameter criteria to enhance decision-making.

However, while useful, these manual charting methods often lead to miscalculations, delays in documentation, and inconsistent adherence to escalation protocols. The manual process of recording on a standard paper NEWS chart as seen in Figure 2 is a four-step process:
- capturing each of the observed values used in the NEWS assessment
- plotting each value within the range of values specified on the chart
- reading across to determine the risk score for each observation
- summing-up each observation risk score to record an overall NEWS.
Each step in the process is prone to human error that may result in an incorrect NEWS record. These inefficiencies could negatively impact patient outcomes. To address these short-comings, digital EWS systems have become increasingly common, automating the calculation process using real-time data entered by staff. These systems display information on bedside monitors, mobile devices, or nursing station dashboards, enabling clinicians to quickly assess patient acuity and make informed decisions.
Taking Steps towards EWS Digitization
Digitizing EWS: A two-step process:
- Digital Spot Aggregation: Initially, manual spot-checks were digitized, allowing staff to record vital signs using mobile devices and allow the system to automatically calculate the NEWS scores. This provided a more consistent and streamlined data collection process that improved both accuracy and speed.
- Continuous Data Monitoring: Building on this, continuous monitoring through the use of wearables and sensors has been proposed as a method for early detection of abnormal signs in patients on general wards, with the goal of replacing traditional intermittent measurements. Continuous monitoring allows healthcare professionals to detect subtle trends in vital signs that might otherwise be missed during periodic checks. For instance, in certain cases, trends in nighttime respiratory rates and heart rates can signal deterioration earlier than spot measurements. However, in such automated systems, nurses are unable to validate abnormal vital signs as they usually would and this can lead to an increase in false alarms that are in fact non-actionable. Algorithms are increasingly being developed to address such problems and enhave the sensitivity and specificity of such alarm systems for the identification of patient deterioration using NEWS.
The Shift to Wearables and Automated Monitoring
While the digitization of EWS has made patient monitoring more efficient, the next significant leap will be the integration of wearable technology. Wearables have the potential to replace manual spot measurements entirely, offering continuous, automatic monitoring of patients' vital signs. These devices would collect data in real-time, seamlessly integrating with existing digital EWS systems to provide a more dynamic and responsive approach to patient care. One significant advantage of wearables is the ability to track trends over time, compensating for gaps in manual monitoring. For example, trends in heart rate and respiratory rate during the night can offer valuable insights into a patient’s condition, reducing the need for constant spot checks. Additionally, future EWS systems may be individualized according to each patient, taking into account baseline parameters like sex, age, hospital ward, and medical history to offer more precise risk assessments.
What's Next?
As we look ahead, the convergence of digital EWS and wearable technology represents the future of patient monitoring. In our next article, we’ll explore the exciting role of wearables in healthcare and how they could enhance future early warning scores.
Zitierung des Beitrags
Leifke, M., Geissmann, L. & Wehrli, S. (2025). How can early warnings score improve care? In Flagshipprojekt SHIFT. Wissensbeitrag B.1 (Nr. 2).

